Article by Ariel Helms and Al Powers, MD
WHAT DOES THE PANCREAS DO?
The Pancreas
Sitting below the liver and behind the stomach, the pancreas is nestled into the first section of the small intestine. The banana-shaped pancreas is really two organs in one, and each with a separate function. First, the pancreas is essential for digesting and absorbing foods, including proteins, carbohydrates, and fats. The second function is to produce hormones which regulate blood glucose levels and protein/fat metabolism. Glucose is sugar from the foods we eat, which the body then uses for energy.
The Exocrine Pancreas
Another way to refer to the pancreas’ first job—breaking down foods—is exocrine function. Exocrine glands release chemicals and proteins through ducts. Exocrine tissue makes up over 98% of the pancreas. The exocrine pancreas releases digestive enzymes into the pancreatic duct. The pancreatic duct is a tube-like structure that connects the pancreas to the small intestine where the small intestine branches from the stomach. Once in the small intestine, these digestive enzymes assist with digestion, so that the body can better absorb consumed food for energy. Without these exocrine enzymes, food is not digested properly, which may lead to abdominal pain and diarrhea, especially after meals.
The Endocrine Pancreas
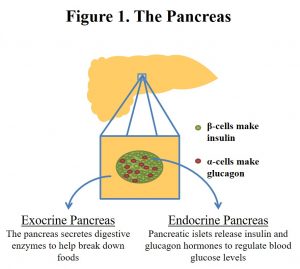
Regulation of blood glucose levels is the pancreatic islet’s endocrine function. Endocrine tissues release hormones directly into the blood stream where they circulate throughout the body and communicate with other tissues. The endocrine pancreas is composed of clusters of hormone-secreting cells called islets, which make up only 1-2% of the pancreas. Islets are composed of different cell types including beta cells and alpha cells (figure 1). Beta cells release the hormone insulin into the blood stream and alpha cells release the hormone glucagon. Beta cells and alpha cells respond to changes in blood glucose in a matter of minutes by releasing the necessary hormones. Although accounting for a very small portion of pancreatic tissue, the endocrine tissue plays a critical role in health.
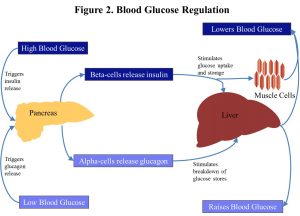
When the level of blood sugar, or blood glucose, rises—such as after eating—beta cells in the pancreatic islets release insulin to lower the blood glucose. Insulin signals to liver, muscle, and other tissues to take in glucose from the blood stream. These tissues will then either use the glucose or store it for later use (figure 2).
If the blood glucose drops too low, the alpha cells in the pancreatic islets release glucagon to raise the blood glucose. Glucagon signals to the liver to break down glucose stores and release it into the blood stream (figure 2).
Without the release of these hormones, blood glucose levels become unstable, as with diabetes. Diabetes is hyperglycemia, or elevated blood glucose, and it can lead to dizziness, fatigue, thirst, and headaches. There are several types of diabetes, including the type associated with pancreas removal. Lower blood glucose, or hypoglycemia, causes shakiness, hunger, sweating, and irritability.
HOW CAN MEN AFFECT THE PANCREAS?
Reasons for Pancreatic Removal
Tumors in the pancreas are sometimes treated by surgical removal of the tumor and its surrounding tissue. Patients with Multiple Endocrine Neoplasia (MEN) are predisposed to the development of pancreatic endocrine tumors that are usually benign, but can be malignant. Depending on a variety of factors, tumors are sometimes treated by removal of a part of the pancreas or the entire pancreas (pancreatectomy). In a partial pancreatectomy, the tumor-containing section is surgically removed. In a total pancreatectomy, the entire organ is removed. A total pancreatectomy may be required in cases with a large tumor to ensure that all tumor tissue is removed.
WHAT HAPPENS AFTER A PANCREATECTOMY?
Pancreoprivic Diabetes
If a majority of pancreatic tissue is removed, medication is required to replace both pancreatic functions. Usually, up to 50 percent of the pancreas can be removed without resulting in diabetes. Depending on how much of the pancreas is removed in a partial pancreatectomy, close monitoring of blood glucose levels and eating habits is necessary and medication may be needed to aid in the pancreas’ partial loss of function. After removal of the entire pancreas, the body loses its ability to regulate blood glucose levels and to assist in digestion.
Replacing Pancreas Endocrine Function
Without the pancreas, the body cannot regulate blood glucose. This is called pancreoprivic diabetes. Pancreoprivic diabetes is an especially challenging form of diabetes. Unlike type 1 or type 2 diabetes, in which the insulin-producing beta cells are destroyed or do not function properly, pancreoprivic diabetes is also associated with a loss of exocrine function and requires insulin to replace endocrine function. Insulin can be delivered either through injections or with an insulin pump, which gradually delivers insulin.
Patients with pancreoprivic diabetes should eat regularly and keep track of what they eat. Prior to meals, patients give themselves an insulin dose that corresponds to the amount of sugar in their meal. Insulin may take several hours to act completely. Patients must check their blood glucose frequently in order to determine how much insulin is needed. When blood glucose becomes too low, patients should eat or take glucose tablets, which are absorbed more quickly, to raise their blood glucose level. Extreme hypoglycemia may cause seizure or coma. If a patient has hypoglycemia and cannot eat, glucagon injection is necessary to raise the blood glucose.
Replacing Pancreas Exocrine Function
The body relies on the pancreas to provide enzymes that help digest fatty foods and proteins. After removal of the pancreas, the body also loses its ability to digest food. Patients whose pancreas has been removed must take pancreatic enzyme pills, which contain some of these missing enzymes, to replace the exocrine function of the pancreas.
Conclusion
Living without a pancreas requires very careful attention to blood glucose levels and disciplined use of insulin therapy and pancreatic enzyme pills. Although pancreoprivic diabetes is challenging, it can be successfully managed with proper medical care and careful attention to one’s body.
Click here to download this article and related images as a PDF resource

Leave a Reply